loading...

by Tim Cassidy | Jul 23, 2024 | Educational
According to Jenner Law firm, the most common violations in therapy include sexual relations, breach of confidentiality, and engaging in dual relationships.
For this reason, continuing education in ethics for therapists enables them to protect their clients and profession. Also, ethics CEUs (Continuing Education Units) allow you to grow professionally and strengthen your practice’s integrity.
In this blog post, we’ll dive into the significance of CEUs in ethics, their impact on your career, and how they contribute to mental health practices.
What Are the Ethical Considerations for Therapists?
Ethical principles are a framework that helps therapists make decisions based on fairness, respect, and responsibility. They guide you on how to serve your clients best and protect yourself from potential legal or professional repercussions.
And they include confidentiality, dual relationships, informed consent, and professional boundaries.
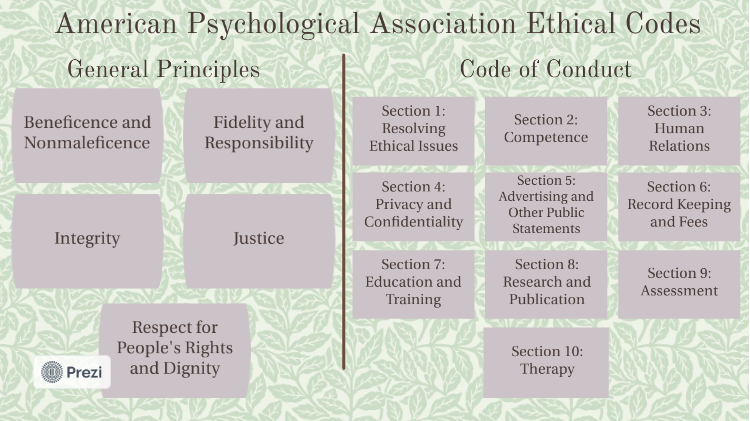
For example, the American Psychological Association’s Ethical Principles of Psychologists and Code of Conduct provide guidelines for psychologists to consider when making decisions about their clients.
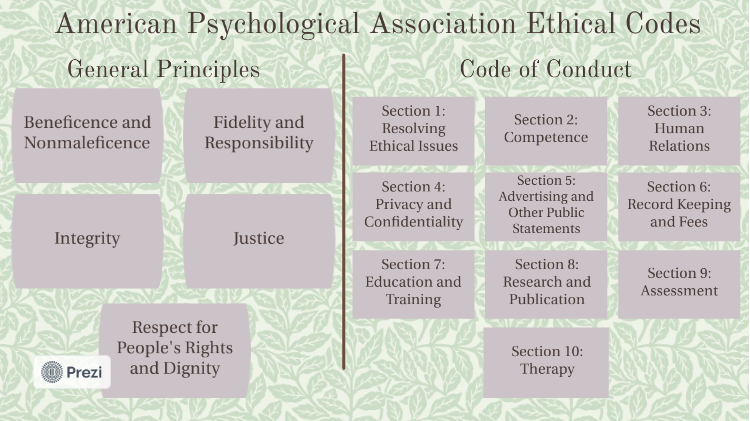
Image Source
Ethics for counselors enable you to navigate complex situations where the lines between right and wrong might blur. So adhering to ethical principles protects your clients, upholds the profession’s integrity, and maintains public trust.
Why Does Ethics Matter in Mental Health Practice?
Ethics form the backbone of any professional practice, and this is especially true in mental health. As a therapist, counselor, social worker, or psychologist, you have a delicate and significant responsibility to guide individuals through their most vulnerable moments.
Your decisions and actions can profoundly impact their lives. This is why understanding and adhering to ethical standards are non-negotiable.
What’s the Role of Ethics CEUs?
Ethics CEUs keep you updated on the latest ethical standards and practices in mental health. They’re not just a box to check off on your license renewal form, but a crucial aspect of your professional development. Ethics courses provide you with the tools and knowledge to handle ethical dilemmas with confidence and competence.
Continuing education in ethics helps you stay current with changes in laws and regulations affecting your practice. You learn about new ethical challenges that might arise due to technological advancements, changes in societal norms, or clinical practice developments.
For instance, the rise of telehealth and other therapeutic technologies has introduced new ethical considerations regarding confidentiality and client privacy. Ethics CEUs can help you manage these new terrains effectively.
Enhancing Professional Competence
One of the key benefits of ethics CEUs is that they enhance your professional competence. These courses involve case studies, real-life scenarios, and interactive discussions that challenge you to think critically about ethical issues.
Also, they encourage you to reflect on your own practices and identify areas where you need to improve. As a result, you understand ethical principles in-depth and learn how to apply them in your daily practice.
Ultimately, CEUs in ethics let you make better decisions and boost your confidence in handling complex ethical situations. It reassures your clients about your commitment to maintaining the highest standards of professional conduct.
Building Trust with Clients
Trust is the foundation of any therapeutic relationship. Clients must feel confident that you’re trustworthy, competent, and committed to their well-being. You demonstrate your dedication to ethical practice and professional growth when you engage in ethics CEUs.
The programs can boost your reputation and help you build stronger relationships with your clients.
In addition, patients can trust you with their personal and sensitive information when they know you’re continuously educating yourself on ethical issues.
They can get assurance that you’ll handle their cases with the utmost care and integrity. And this trust is vital for effective therapy and positive outcomes.
Navigating Ethical Dilemmas
Ethical dilemmas are an inevitable part of mental health practice. Whether it’s maintaining confidentiality when a client poses a danger to themselves or others, managing dual relationships, or ensuring informed consent, ethical challenges can arise unexpectedly.
So ethics training programs can equip you with the knowledge and skills to cope with these dilemmas effectively.
Also, they present complex scenarios that require you to think critically and make tough decisions. The courses provide a safe space to explore different perspectives and outcomes, helping you prepare for real-life situations.
You can approach dilemmas with greater clarity and confidence by honing your ethical decision-making skills.
Staying Updated with Regulatory Changes
Mental health is evolving, with new research, technologies, and regulations emerging regularly. Keeping up with these changes allows you to maintain your license and provide the best possible care for your clients. CEUs in ethics let you stay informed about new laws and guidelines that impact your practice.
For example, changes in confidentiality laws, mandatory reporting requirements, or telehealth regulations can affect how you conduct your practice. Completing ethics CEUs keeps you updated on these changes, helping you remain compliant and avoid legal pitfalls.
Promoting a Culture of Ethical Practice
As a result of ethics CEUs, mental health experts can contribute to a culture of ethical practice throughout the profession.
When you prioritize ethical education, you can set a standard for your peers and colleagues. And this collective commitment to ethics enhances the profession’s reputation.
You can also become a role model for others in your career by going through ethics programs. This fosters a culture of continuous learning and ethical awareness, ultimately benefiting clients and the profession.
How To Choose the Right Ethics Programs
The next step is selecting the right courses to fulfill your continuing education requirements. Not all CEUs are created equal, so pick high-quality, reputable courses that provide valuable content and meet your state’s requirements.
Look for accredited courses from recognized organizations, such as the American Psychological Association (APA) or the National Association of Social Workers (NASW). The certifications enable you to meet the licensing boards’ standards and offer relevant, up-to-date information.
Consider the format of the courses as well. Online courses offer flexibility and convenience, allowing you to complete your CEUs at your own pace and from the comfort of your home or office. And they’re perfect for busy professionals who want to balance their education with their practice.
Protect Your Clients and Profession with Ethics Courses

Courses in ethics are like an insurance policy, which protects and empowers you to provide the best possible services to your clients. For this reason, Online CE Credits is a therapist-managed training platform with in-depth and on-demand ethics CEUs. It offers over 250 programs online from established therapists to allow you to study anytime, anywhere.
Ready to kickstart your ethics courses? Select from the accredited programs below:
How To Make the Most of Your Ethics CEUs
To get the most out of your CEUs in ethics, approach them with an open mind and a willingness to learn. Engage actively in the course material, participate in discussions, and reflect on how the concepts apply to your practice.
Also, consider keeping a journal to document your thoughts and insights, which’ll serve as a valuable resource for future reference.
Don’t hesitate to seek out additional resources or mentorship if you encounter ethical dilemmas that you find challenging. Discussing these issues with colleagues or supervisors can provide new perspectives and help you develop a more nuanced understanding.
Explore Ethics for Therapists
Remember, ethics CEUs are not just a requirement but an opportunity for growth. Embrace them to hone your professional skills, improve practice, and better serve your clients. Also, integrating ethics into your continuing education demonstrates your commitment to excellence and integrity.
In addition, ethics programs keep you updated on the latest ethical standards, advance your professional competence, and build trust with your clients. They equip you with the knowledge and skills to handle ethical dilemmas and maintain the highest standards of professional conduct.
Fuel Your Success with Nationally Approved Ethics Courses
If you’re looking for accredited programs in ethics for counselors, psychologists, social workers, or mental health professionals, you’re on the right platform. Online CE Credits provides nationally approved ethics CEUs to help you advance your career and fulfill licensure requirements. The best part? You can gain instant access to the lessons at affordable rates.
Don’t take our word for it. Stop just meeting the minimum requirements. Get the knowledge and skills to become a leader in ethics courses.
FAQS
What is the Universal Declaration of Ethics for psychologists?
The Universal Declaration of Ethics for Psychologists is a document that provides ethical guidelines for psychologists. It was developed by the American Psychological Association in 1953.
What happens if a psychologist breaks the code of ethics?
If a psychologist breaks the code of ethics, their professional organization may discipline them. This could include being fined, suspended, or having their license revoked. Additionally, they may be held liable for any damages caused to a client or the public.
What are the responsibilities of a psychologist in ethics?
A psychologist must follow the American Psychological Association’s code of ethics, which outlines their responsibilities to their patients, the public, and the profession. These responsibilities include providing competent and ethical care, maintaining confidentiality, and engaging in research that is in the public interest.
What are the violations of ethics in therapy?
Violations of ethics in therapy include engaging in sexual relationships with clients, providing inaccurate or misleading information, and exploiting clients for personal gain.

by Tim Cassidy | Oct 11, 2024 | Educational
Narrative Exposure Therapy (NET) is an evidence-based approach that offers a structured yet flexible way of helping individuals process trauma. As a mental health professional, adding NET to your skill set can provide substantial benefits to your trauma care practice. It’s ideal for clients with complex trauma histories, such as refugees, survivors of war, or individuals with chronic childhood abuse.
NET is grounded in storytelling, encouraging clients to narrate their life experiences within a chronological structure. This not only helps them organize traumatic memories but also aids in integrating those experiences into their broader life narrative.
Understanding the NET Approach
In many trauma-focused therapies, the goal is to help clients reprocess traumatic events to reduce symptoms of PTSD and other related conditions. NET takes a unique approach by focusing on creating a coherent autobiographical timeline of the client’s life. The client is encouraged to explore both positive and traumatic experiences, situating their memories within their overall life story.

NET follows a structured format where clients recount their memories in chronological order, focusing particularly on the most intense or distressing events. This helps clients face traumatic memories while emphasizing that these events are part of a larger, more complex life narrative. Through this process, NET seeks to transform fragmented, disorganized memories into a more cohesive story.
The therapist guides the client through this journey, helping them not only recount their trauma but also place it within the broader arc of their lives. This allows for both emotional processing and cognitive restructuring, helping individuals understand their trauma as just one part of their life experience rather than the defining feature.
Why NET Is Effective for Trauma Treatment?
NET’s effectiveness lies in its simplicity and focus on narrative coherence. Many clients who experience complex trauma struggle with fragmented memories and disorganized thoughts about their past. So storytelling helps to bridge these gaps. By encouraging clients to recall events in order, the therapy supports emotional processing in a way that makes the memories less overwhelming.
From a neurological standpoint, NET helps by reducing the emotional charge of traumatic memories. Over time, retelling these memories in a safe therapeutic environment can make them less distressing and intrusive. This process helps to reduce symptoms of PTSD, such as flashbacks, nightmares, and hyperarousal.
Additionally, NET promotes resilience by highlighting the client’s strengths and positive memories. When trauma dominates a person’s mind, it’s easy for them to overlook positive aspects of their life. NET encourages clients to remember and integrate these positive experiences, which can enhance their overall emotional well-being and self-worth.
How NET Fits Into Trauma Care
One of the key benefits of NET is its structured yet adaptable format. If you’re used to trauma-focused approaches like Cognitive Behavioral Therapy (CBT) or Eye Movement Desensitization and Reprocessing (EMDR), you might find NET to be a valuable addition to your toolbox. It works with clients who have multiple, layered trauma experiences.
One of the core principles of NET is that it’s helpful for individuals who have experienced ongoing, repeated trauma. Many therapies, while effective, are more suited for single-event trauma. NET, by contrast, is well-suited to clients who have been exposed to prolonged trauma, such as survivors of conflict, forced migration, or childhood abuse. By organizing these experiences into a timeline, the therapy allows for the processing of multiple traumatic events, giving clients a sense of control over their past.
The Process of Becoming Trained in NET
If you’re interested in incorporating NET into your practice, training is accessible and can often be completed over the course of a few days. The training typically covers the basic principles of the therapy, including how to structure sessions, work with traumatic memories, and create the life narrative with your client.
The initial training gives you the foundational skills to begin using NET in your practice, but many professionals choose to continue refining their skills through supervision or advanced workshops.
A particularly valuable aspect of NET training is the focus on cultural competence. Given that NET has been used extensively with refugees and survivors of war, the training often emphasizes how to work with clients from diverse cultural backgrounds. This makes it especially useful for therapists who work in multicultural settings or with clients from marginalized populations.
Real-World Application: Bringing NET Into Your Practice
Once trained, many therapists find that NET can complement other forms of trauma therapy. For example, if you’re working with a client who struggles to make sense of their traumatic experiences, incorporating NET can provide a way to organize those memories into a more coherent whole.

The therapy can be especially useful for clients who find it difficult to talk about their trauma in detail, as the structured nature of NET provides a sense of containment and safety.
Many therapists also report that NET helps improve therapeutic rapport. By working with clients to tell their story, therapists can foster a sense of collaboration and mutual trust. This can be particularly helpful when working with clients who have had difficulty opening up in other therapeutic settings.
Incorporating NET into your practice doesn’t mean you need to abandon other techniques you use. Many professionals find that NET works well alongside other therapies, such as EMDR or Trauma-Focused Cognitive Behavioral Therapy (TF-CBT). For instance, you might use NET to help a client organize their traumatic memories and then use EMDR to process particularly distressing memories in more depth.
The flexibility of NET allows it to be adapted to your specific clinical style and the unique needs of your clients. For those working in community mental health settings or with underserved populations, NET can be especially useful because it is designed to be brief and effective even in low-resource settings. This makes it an ideal choice for therapists who may not have the luxury of long-term therapeutic interventions with their clients.
Expanding Your Trauma Care Practice With NET
Expanding your skill set to include NET opens up new opportunities for working with diverse populations. Whether you’re working in private practice, a community clinic, or a humanitarian setting, NET provides a structured and effective way to help clients process trauma. The emphasis on narrative allows clients to reclaim their story, offering a sense of agency and control that is often lost in the aftermath of trauma.
NET also offers a powerful way to help clients integrate their experiences into a coherent and manageable narrative. By incorporating this therapy into your practice, you can offer a more structured, client-centered approach to trauma care that addresses both the emotional and cognitive aspects of trauma. For clients who have been through significant, complex traumas, this approach can make a world of difference in their journey toward healing.

by Tim Cassidy | Oct 11, 2024 | Educational
Solution-Focused Therapy (SFT) is a strengths-based approach that helps clients envision their preferred future and identify the steps needed to achieve it. Unlike some therapeutic methods that focus heavily on analyzing problems, SFT shifts the focus to solutions, resources, and the client’s existing strengths. This method often proves effective for clients who want to make tangible progress in a relatively short time.
Get up to speed with SFT to hone your skills and earn 2.5 credits effortlessly.
Let’s explore several essential SFT questions that drive client engagement and facilitate meaningful change.
The Miracle Question: Envisioning the Future
The Miracle Question is perhaps one of the most well-known tools in SFT. It invites clients to imagine a future where their issues are resolved overnight. This technique helps clients articulate their goals and desires, often in ways they hadn’t previously considered.

“Suppose tonight, while you sleep, a miracle happens and the problem that brought you here is resolved. How would you know that a miracle happened? What would be different?”
This question can help clients shift from a problem-focused mindset to one that is more solution-oriented. They start to visualize a future where they have overcome their current challenges, which can be incredibly empowering.
Scaling Questions: Measuring Progress and Confidence
Scaling questions are used to assess a client’s current position relative to their goals and to identify small, achievable steps for moving forward. These questions are particularly useful for tracking progress over time and for making abstract concepts more concrete.
“On a scale from 0 to 10, where 0 means the problem is the worst it has ever been and 10 means the problem is completely resolved, where do you see yourself today?”
Follow-up questions like, “What would it take to move one step up the scale?” encourage clients to think about specific, manageable actions to improve their situation. Scaling questions not only help in setting realistic goals but also provide a framework for celebrating small victories along the way.
Exception Questions: Discovering What Works
Exception questions help clients identify times when their problem was less severe or when they were able to cope more effectively. These questions are vital for uncovering hidden strengths and resources that the client can use in the present.
“Can you think of a time recently when the problem wasn’t as intense? What was different about that situation?”
By pinpointing these moments, clients can begin to understand what factors contributed to their success during those times. Whether it’s a supportive friend, a particular mindset, or a coping strategy, identifying these exceptions can be key to replicating and building upon past successes.
Coping Questions: Acknowledging Effort and Resilience
Coping questions are particularly helpful for clients who feel stuck or overwhelmed. These questions acknowledge the effort the client is already putting in and validate their ability to manage difficult situations, even if they aren’t seeing significant changes yet.
“How have you managed to keep going, despite the difficulties you’re facing?”
This type of question can open up a discussion about the client’s resilience and the small, perhaps unnoticed ways they are already coping. It shifts the focus from what isn’t working to what is, no matter how small or seemingly insignificant.
Goal-Oriented Questions: Defining Success
Setting clear, concrete goals is a cornerstone of SFT. Goal-oriented questions help clients articulate what they want to achieve in a way that is specific and actionable. This clarity is crucial for both the client and the therapist to work effectively towards achieving those goals.
“What will be the first sign that things are getting better for you?”
This question encourages clients to define success in their own terms, providing a tangible marker to strive toward. Having a clear indicator of progress helps in maintaining motivation and focus throughout the therapeutic process.
Exploring Motivation: What’s at Stake?
Understanding what motivates a client to seek therapy is crucial for tailoring the therapeutic approach to their needs. Questions that explore motivation can help both the therapist and the client understand the deeper reasons for wanting change, which can be pivotal in sustaining effort and engagement.
“What makes this change important to you right now?”
This question can reveal underlying values and priorities, making it easier to align therapeutic interventions with what the client truly cares about. Whether it’s family therapy, personal well-being, or career aspirations, identifying these motivators can significantly enhance client commitment to the process.
Resource Questions: Uncovering Hidden Strengths
Resource questions aim to uncover the internal and external resources the client already possesses. These could be personal traits, supportive relationships, or past experiences that have equipped them to handle challenges.
“When you’ve faced difficulties like this before, what helped you get through it?”
By identifying these resources, clients can begin to see themselves as more capable and resilient. This recognition can be empowering and can serve as a foundation for developing new coping strategies and solutions.
Exploring Small Steps: Incremental Change
Sometimes the path to change can feel overwhelming, and clients may struggle to see how they can get from where they are to where they want to be. Exploring small, actionable steps can make the process feel more manageable.
“What’s the smallest step you can take this week that would move you closer to your goal?”
This question helps clients break down their goals into smaller, more achievable tasks. Taking incremental steps can build momentum and provide a sense of accomplishment, which is crucial for maintaining motivation over time.
Strengths-Based Questions: Highlighting What’s Working
Clients often come to therapy feeling discouraged and may have a negative view of themselves. Strengths-based questions help shift this narrative by highlighting the client’s skills, attributes, and past successes.

“What qualities or strengths have helped you navigate tough times before?”
Acknowledging these strengths can help clients build a more positive self-concept and foster a sense of self-efficacy. This can be particularly important for clients who struggle with low self-esteem or who have difficulty recognizing their own accomplishments.
Future-Oriented Questions: Visualizing the Path Ahead
Future-oriented questions help clients imagine what life could look like once they’ve achieved their goals. This vision can serve as a powerful motivator and provide a sense of hope and direction.
“How will your life be different once you’ve achieved your goals?”
Encouraging clients to think about the positive changes they want to see can help maintain focus and motivation. It also provides a concrete picture of what they are working towards, making the therapeutic process feel more purposeful and directed.
Conclusion: Master SFT Questions To Dominate Your Practice
Incorporating these essential questions into your SFT practice can significantly enhance client engagement and facilitate meaningful progress. Each question serves a distinct purpose, whether it’s helping clients articulate their goals, recognize their strengths, or take actionable steps toward change.
By fostering a collaborative, solution-focused dialogue, therapists can empower clients to become active participants in their own healing process. It can be a valuable tool whether you are new to Solution-Focused Therapy or looking for ways to deepen your practice. Advance your career today and dominate your practice.

by Tim Cassidy | Sep 27, 2024 | Educational
Intergenerational trauma is not just a passing concern for many mental health professionals. It’s a persistent challenge that can span several generations, affecting families, communities, and entire cultures. Whether stemming from war, systemic oppression, or family violence, this trauma can influence how people relate to each other, how they parent, and how they navigate their personal and social lives.
Recognizing these deep-rooted patterns, the Intergenerational Trauma Treatment Model (ITTM) has been developed to address the needs of those affected, offering a path toward healing and recovery.
The Reality of Intergenerational Trauma
The concept of intergenerational trauma is not new. It refers to the transmission of trauma from one generation to the next. Trauma doesn’t just affect the person who directly experienced it; it can seep into family dynamics, parenting styles, and even genetic makeup.
Trauma survivors’ children often grow up in environments shaped by the emotional and psychological wounds of their parents, even if the original trauma occurred decades ago.

For example, children who have grown up in families affected by slavery or genocide often exhibit signs of trauma, even without direct exposure to the events themselves. The trauma can manifest in a variety of ways, such as anxiety, depression, difficulties in forming relationships, or a pervasive sense of fear or distrust.
This kind of trauma is complex because it’s often intertwined with cultural, historical, and familial contexts, making it challenging to treat through traditional methods.
Embrace Several Therapy Interventions To Treat Intergenerational Trauma
Mental health professionals such as psychiatrists, psychologists, and other physicians are concerned about the effect of intergenerational trauma. So does Online CE Credits, a therapist-managed platform with the most up-to-date trauma treatments. The online courses empower you to apply emerging trauma techniques to help your clients heal.
Take a look at the accredited courses below:
The Need for a Specialized Treatment Approach
Intergenerational trauma requires a specialized approach that goes beyond individual therapy. While traditional therapy can address personal experiences of trauma, it may fall short in recognizing and treating the ways trauma is passed down through families and communities.
The ITTM is designed specifically to address these unique challenges by focusing not just on the individual but also on their family and community context.
The model acknowledges that healing needs to occur on multiple levels. It’s not enough to address the trauma in the person sitting in the therapist’s chair. Instead, ITTM seeks to understand the broader picture—how family dynamics, community relationships, and cultural histories all contribute to the perpetuation of trauma.
The goal is to break the cycle of trauma transmission and help individuals and families create new, healthier patterns.
Core Components of the Intergenerational Trauma Treatment Model
The ITTM integrates several therapeutic approaches to provide a comprehensive treatment plan. These include:
Family Therapy:
Since trauma often affects entire families, therapy sessions that include multiple family members can be crucial. Family therapy within the ITTM framework helps families understand the origins of their struggles and how trauma has influenced their relationships.
This kind of therapy is vital for uncovering and addressing unhealthy patterns that may have been passed down from generation to generation.
Narrative Therapy:
Encouraging individuals and families to share their stories is a powerful tool in the healing process. Narrative therapy allows people to reframe their experiences, helping them see themselves not as victims of their past but as survivors with the strength to create a different future.
This aspect of ITTM is particularly important for communities where silence and secrecy around trauma have been prevalent, giving voice to those who have been historically silenced.
Cultural Sensitivity:
The ITTM recognizes that culture plays a significant role in how trauma is experienced and transmitted. Treatment plans are therefore tailored to respect and incorporate cultural beliefs and practices.
This can involve working with community leaders, understanding cultural rituals and traditions, and acknowledging the specific historical and cultural contexts that have contributed to the trauma.
Psychoeducation:
Educating clients about the nature of trauma and its effects is a fundamental part of ITTM. Understanding how trauma impacts the brain, body, and behavior can be incredibly empowering for clients. This knowledge helps them make sense of their experiences and realize that their reactions are normal responses to abnormal circumstances.
Interventions for Children and Adolescents:
Children and adolescents who grow up in traumatized environments need age-appropriate specialized interventions sensitive to their developmental stages. ITTM includes strategies such as play therapy, art therapy, and trauma-focused cognitive-behavioral therapy (TF-CBT) to help young people process their experiences in a safe and supportive environment.
Community-Based Approaches:
Healing doesn’t happen in isolation. ITTM often involves community-based approaches that foster a sense of belonging and collective healing. This can include group therapy sessions, community workshops, and cultural healing practices that bring people together to share their experiences and support one another.
The Role of Therapists in ITTM
Therapists working within the ITTM need to be particularly attuned to intergenerational trauma’s complex dynamics . This requires them to combine clinical expertise, cultural competence, and a deep understanding of family systems. Health professionals must be able to hold space for clients as they explore painful and often deeply buried emotions.
They also need to be skilled in helping clients recognize and disrupt unhealthy patterns of behavior that have been passed down through generations.
Also, practitioners must be aware of their own potential biases and the ways in which their own cultural backgrounds may influence their understanding of trauma. Continuous training and supervision are essential for therapists working with intergenerational trauma to ensure they provide the most effective and sensitive care possible.
Challenges and Considerations in ITTM
While ITTM offers a promising approach to healing intergenerational trauma, it’s not without its challenges. One of the primary difficulties is the deeply entrenched nature of intergenerational trauma. Breaking the cycle requires not just time and effort but also a willingness to confront painful family histories and cultural legacies. This process can be emotionally exhausting for both clients and therapists.
In addition, factors such as the availability of culturally competent therapists, access to resources, and the level of support within the community can influence ITTM’s effectiveness. In some cases, there may be resistance to addressing trauma, particularly in cultures where discussing such issues is taboo.
Overcoming these barriers requires a sensitive and patient approach, as well as a strong commitment to the long-term process of healing.
Moving Forward: The Future of Intergenerational Trauma Treatment
The Intergenerational Trauma Treatment Model represents a significant step forward in our understanding of how trauma is transmitted across generations and how it can be treated. ITTM breaks the cycle of trauma transmission by addressing trauma on multiple levels—individual, family, and community—and paves the way for a healthier, more resilient future.

Mental health professionals working with intergenerational trauma require a deep commitment to learning, cultural sensitivity, and ongoing professional development. As our understanding of trauma continues to evolve, the ITTM will likely continue to adapt and grow, incorporating new research and therapeutic techniques.
However, what remains constant is the model’s emphasis on healing individuals, families, and communities.
Consider ITTM To Treat Complex Trauma
The ITTM is not just a treatment model—it’s a pathway to healing that honors the complex and multifaceted nature of trauma. Intergenerational trauma survivors have hope for a future without the burden of their past.
And therapists can use the model to make a profound difference in their clients by helping them break free from trauma cycles that have held them captive for far too long.
Want to fine-tune your trauma interventions? Partner with Online CE Credits by creating an account today.

by Tim Cassidy | Sep 27, 2024 | Educational
Living with anxiety and depression can often feel like navigating through a maze without a clear exit. These conditions can dominate one’s life, making even simple tasks feel overwhelming. For many, finding a therapy that offers a sense of hope and actionable steps forward can make a significant difference.
Solution-focused therapy (SFT) is one such approach that provides a more positive and forward-looking perspective. It focuses on what clients want to achieve rather than what they want to eliminate. This subtle shift can have profound effects on those struggling with anxiety and depression.
Need to jumpstart your continuing education? Consider a nationally approved SFT course.
What Sets Solution-Focused Therapy Apart?
Unlike many traditional therapies that focus on diagnosing and analyzing past experiences, SFT is a short-term, goal-oriented therapeutic approach. It emphasizes solutions and the future rather than delving into the past. This approach can be particularly helpful for those with anxiety and depression, as it helps clients envision a life beyond their current struggles.

SFT revolves around the belief that clients already possess the strengths and resources needed to overcome their difficulties. The therapist’s role is to help the client identify and build on these strengths. You can achieve this by asking specific, targeted questions to encourage clients to think about what they want their future to look like. These are known as “miracle questions,” and they invite clients to imagine how their lives would be different if their problems were resolved.
Real-Life Application in Treating Anxiety and Depression
To see how SFT works in practice, consider a client named Sarah, who has been dealing with severe anxiety. She constantly worries about things going wrong at work, in her personal life, and even in situations she has no control over. In a traditional therapeutic setting, Sarah might spend many sessions exploring the root causes of her anxiety. But in SFT, the therapist might instead ask Sarah to describe a day when she doesn’t feel anxious. What would she be doing? How would she be feeling?
This type of questioning does two things: it shifts the focus from the problem to the solution, and it empowers the client to think about positive changes. For Sarah, this might mean recognizing that on days when she feels less anxious, she spends time outdoors, talks to supportive friends, or engages in hobbies she enjoys. The therapist can then work with Sarah to incorporate these activities into her daily routine, building a foundation for reducing her anxiety.
Emphasizing Small, Achievable Goals
One of the hallmarks of SFT is its emphasis on small, manageable goals. Depression, in particular, can sap motivation, making even minor tasks seem insurmountable. By setting small, achievable goals, clients can begin to experience success and build momentum.
Take the case of John, a client struggling with depression. John finds it hard to get out of bed most days, let alone go to work or socialize. An SFT practitioner might work with John to set a simple goal like getting out of bed at a specific time every day, or taking a short walk each morning. These goals are small but significant steps forward. As John accomplishes these tasks, he gains a sense of achievement and control, which can help combat the feelings of helplessness that often accompany depression.
Building on Exceptions
Another useful aspect of SFT is the identification of “exceptions.” These are times when the client’s problem is less severe or absent altogether. By exploring these exceptions, clients and therapists can identify what is working and how to replicate it.
For someone experiencing anxiety, an exception might be a day when they felt more relaxed, such as during a vacation or while engaged in a particular hobby. The therapist and client can then explore what made that day different and how similar conditions can be created in everyday life.
Fostering a Collaborative Relationship
In SFT, the therapist and client work together as a team. The therapist doesn’t position themselves as the expert who knows all the answers. Instead, they act as a guide, helping the client find their own solutions. This collaborative approach can be especially empowering for those who feel overwhelmed by anxiety and depression. It shifts the dynamic from “being treated” to “actively participating in change.”
Why SFT May Be a Good Fit for Many
SFT can be a refreshing option for clients who are frustrated with longer-term therapies or those who prefer a more action-oriented approach. Its focus on the present and future rather than the past offers a more hopeful outlook. The goal is to encourage clients to focus on their strengths and abilities instead of their limitations.
Also, SFT is adaptable. It can be used in individual, couple, or family settings and is often effective in combination with other therapeutic approaches. For instance, someone undergoing cognitive-behavioral therapy (CBT) might find that integrating SFT techniques helps them stay focused on their goals and recognize the progress they’re making.
Potential Challenges and Limitations
While SFT has many benefits, it’s not without its challenges. It may not be suitable for those who need to process significant trauma or who are looking for a deeper understanding of their condition. Some clients might initially find it difficult to shift focus from their problems to solutions, especially if they’re accustomed to more traditional forms of therapy.

However, SFT can provide quick, tangible results for those open to trying a different approach. It’s often used as a complement to other therapies rather than a standalone treatment, offering clients additional tools to manage their symptoms.
Integrating SFT into Practice
Mental health professionals can integrate SFT into their practice to help clients with anxiety and depression. Training in SFT can be relatively brief compared to other therapeutic modalities, and many find that the skills learned can enhance their overall therapeutic approach. By asking solution-focused questions and helping clients identify their own resources, therapists can foster a more positive and proactive therapeutic environment.
Embrace SFT To Level Up Your Practice
In summary, while anxiety, grief, and depression can be deeply challenging, solution-focused therapy offers a way to navigate these conditions with hope and clarity. By concentrating on solutions and building on strengths, clients can find a renewed sense of agency and optimism. For many, this shift in focus—from problems to possibilities—can be life-changing. Now is the time to polish your SFT knowledge.

by Tim Cassidy | Sep 27, 2024 | Educational
Therapists have a variety of approaches to choose from when working with clients, each offering unique benefits. Two popular models are Narrative Therapy and Solution-Focused Therapy. While both aim to help individuals improve their lives, they do so in very different ways. Understanding these differences can help practitioners select the most effective approach for their clients’ specific needs.
Want to upskill yourself in Solution-Focused Therapy and earn 2.5 credits from the comfort of your home? Explore more about how you can complete the course in a breeze.
Origins and Philosophy
Michael White and David Epston developed Narrative Therapy in the 1980s. It’s rooted in the idea that people construct their identities through the stories they tell about themselves. These narratives shape how individuals perceive their experiences and interact with the world. The therapist’s role is to help clients re-author their stories, focusing on their strengths and abilities rather than the problems they face.

On the other hand, Steve de Shazer and Insoo Kim Berg pioneered Solution-Focused Therapy (SFT) around the same time. This approach emphasizes creating solutions rather than dwelling on problems. It’s a forward-looking, goal-directed method that encourages clients to envision a preferred future and identify steps to achieve it.
The practitioner works with the client to build on what’s already working, however small or seemingly insignificant those successes might appear.
Approach To Problems and Solutions
A fundamental distinction between the two therapies lies in how they approach problems. Narrative Therapy views problems as separate from the person. It sees issues as being external to the individual, influenced by societal, cultural, and contextual factors.
For instance, instead of saying, “I am depressed,” a client might say, “Depression has taken a hold of me.” This externalization technique helps clients view their problems as challenges that can be overcome rather than as inherent aspects of themselves.
However, Solution-Focused Therapy takes a more direct route by focusing on solutions rather than problems. SFT practitioners often use a technique called the “miracle question,” asking clients to imagine what their life would look like if their problem was suddenly solved.
The approach encourages them to think about small, manageable steps to move toward their desired outcome. In SFT, the problem itself isn’t the focal point; the client’s preferred future is.
Use of Language and Storytelling
Language plays a critical role in both therapies, but in distinct ways. Narrative Therapy involves detailed storytelling. Clients are invited to share their narratives in-depth, which allows them to see the events in their lives from different angles. This process can reveal overlooked strengths or alternative interpretations of difficult situations.
In contrast, Solution-Focused Therapy uses language more strategically to steer conversations toward solutions. Questions are framed to elicit descriptions of past successes, exceptions to the problem, and potential steps forward.
For example, a therapist might ask, “Can you tell me about a time when this issue was less intense or more manageable?” This shifts the focus away from the problem and toward effective strategies that the client may have already employed.
Session Structure
In practice, the structure of sessions also differs significantly. Narrative Therapy sessions tend to be more exploratory, with the therapist and client working collaboratively to explore and reshape the client’s narrative. There is often no fixed agenda; instead, the conversation flows according to the client’s storytelling process.
By contrast, Solution-Focused Therapy is often more structured and brief. The practitioner typically begins by clarifying what the client wants to achieve from the session. Then, they work together to identify small, actionable steps that can lead to improvement. The focus is on making tangible progress in a short period, which is why SFT is commonly used for short-term interventions.
How To Apply the Therapies To Different Client Needs
Narrative Therapy is particularly useful for clients dealing with issues related to identity, trauma, or complex life stories. It provides a space to explore the impact of past experiences and societal narratives on their self-concept. People who struggle with self-blame or feel overwhelmed by their circumstances may find this approach very helpful.
Solution-Focused Therapy can be especially helpful for clients seeking quick relief from specific issues, such as managing anxiety or improving relationships. It’s well suited for individuals who are interested in changing but feel stuck. SFT is also a practical choice for situations where time is limited, such as in school counseling or workplace settings.
The Therapist’s Role
In Narrative Therapy, the therapist takes on the role of a collaborator or co-author. They are not seen as the expert who provides answers but as a guide who helps the client find their own meaning and solutions. By promoting clients as experts in their own lives, this egalitarian perspective can empower them.
On the other hand, Solution-Focused Therapy sees the therapist more as a facilitator. They guide the client in recognizing their own resources and strengths. While still client-centered, the practitioner in SFT may take a more active role in suggesting specific strategies or encouraging particular lines of thought.
Cultural Sensitivity
Both therapies offer culturally sensitive ways of working with clients, but they do so differently. Narrative Therapy’s emphasis on understanding the impact of societal and cultural narratives makes it particularly attuned to issues of oppression, marginalization, and identity. It invites clients to critically examine the broader influences on their personal stories.
Solution-Focused Therapy, meanwhile, is adaptable across different cultural contexts because of its focus on individual solutions rather than pathologizing problems. It does not require extensive exploration of past issues or societal factors. This makes it a more comfortable fit for clients who might find such discussions intrusive or irrelevant.
Combining Both Approaches
While these therapies have distinct methodologies, they are not mutually exclusive. In fact, many therapists integrate elements of both to suit their clients’ needs. For example, a counselor might use Narrative Therapy techniques to help a client externalize and reframe their problem and then employ Solution-Focused strategies to identify actionable steps for change. This flexible approach allows for a more personalized therapeutic experience.
Choosing the Right Approach
Selecting between Narrative Therapy and Solution-Focused Therapy depends largely on the client’s goals, preferences, and the nature of their issues. Narrative Therapy offers a powerful toolset for clients who need to make sense of complex life events like complex trauma or reframe deeply held beliefs. It provides a space for deep reflection and the re-imagining of self-identity.

Solution-Focused Therapy may be the better option for those who are looking for practical, immediate solutions. Its structured, goal-oriented nature enables clients to quickly identify and implement changes. So it’s ideal for short-term work or for clients who are ready to take action but need help identifying where to start.
Consider Your Client’s Needs
Both Narrative Therapy and Solution-Focused Therapy offer valuable approaches for helping clients navigate their challenges and achieve their goals. By understanding the key differences and applications of each, therapists can better tailor their interventions to meet their clients’ unique needs.
Whether re-authoring stories or building on existing strengths, both therapies empower clients to move toward a more fulfilling life. Ready to integrate SFT into your therapy? Create an account now!