by Tim Cassidy | Apr 7, 2025 | Uncategorized
Online CE Credits is thrilled to announce the launch of a groundbreaking new course, “EMDR 2.0 Skills Mastery: Techniques and Practical Applications,” designed to empower therapists with cutting-edge tools to enhance trauma therapy. This course, now available for enrollment, offers mental health professionals an opportunity to deepen their practice and deliver faster, more effective care to clients.

Building on the proven foundation of traditional EMDR (Eye Movement Desensitization and Reprocessing), EMDR 2.0 introduces advanced techniques to accelerate and deepen the processing of traumatic memories. Key enhancements include working memory taxation techniques and client buy-in strategies. These methods, informed by the latest neurobiological research, aim to provide nuanced, impactful treatment for clients with complex trauma.
“EMDR 2.0 represents a significant step forward in trauma therapy,” says Dr. Jennifer Sweeton, course instructor and a renowned trauma psychologist. “We’re equipping therapists with practical, evidence-based strategies to help clients heal more efficiently, even in challenging cases.”
The live webinar is on January 30, 2025, and afterward will be accessible on demand 24/7, offering flexibility for busy professionals. Therapists can earn continuing education credits while learning at their own pace. Online CE Credits encourages clinicians to stay ahead in their field by integrating these innovative techniques into their practice.
For more information and to register, see: https://onlinececredits.com/events/emdr-2-0-advanced-techniques-for-fast-safe-effective-treatment/
by Tim Cassidy | Mar 10, 2025 | Educational, Uncategorized
Introduction
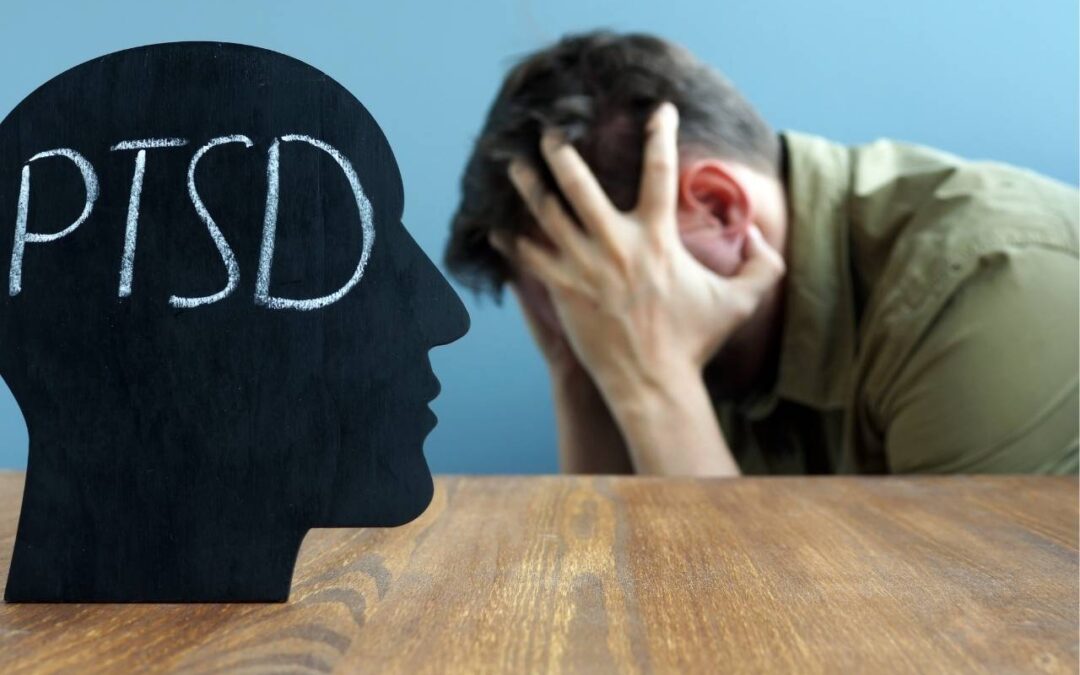
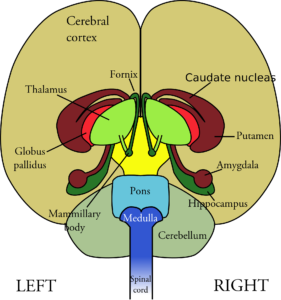
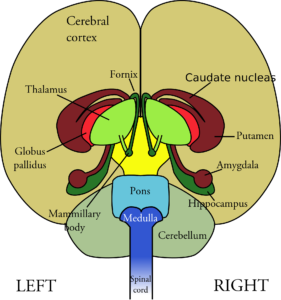
For mental health professionals, understanding the brain can unlock powerful insights into client care. In The Neuroscience Handbook for Clinicians by Dr. Jennifer Sweeton, the thalamus emerges as a critical, often overlooked brain region in trauma therapy. As a “relay station” for sensory information, the thalamus plays a pivotal role in how clients experience PTSD symptoms like re-experiencing and dissociation. Let’s explore its functions, impact on trauma, and how you can apply this knowledge in your practice, and how our CE courses at Online CE Credits can help.
What Is the Thalamus and Why It Matters
The thalamus, a small egg-shaped structure above the brain stem, acts as the brain’s sensory gatekeeper, relaying sensory inputs (except smell) to regions like the amygdala (threat detection) and cortex (executive functioning). That sensory information reaches the amygdala in just 12 milliseconds, which is half the time it takes to reach the cortex (25 milliseconds). This means clients often process danger before rational thought kicks in, a key factor in trauma responses.
The Thalamus in Trauma: Symptoms and Challenges
Research (e.g., Etkin & Wager, 2007; Kim et al., 2007) shows that individuals with PTSD often exhibit thalamic hypoactivation at rest and during re-experiencing symptoms, such as traumatic sensory re-enactments. This reduced activation disrupts sensory filtering, making trauma memories feel vivid and present, as if the event is happening now. And, there is weaker connectivity between the thalamus and amygdala in severe PTSD, exacerbating these symptoms (Zhu et al., 2017). Conversely, during dissociation or flashbacks, the thalamus becomes hyperactive, over-filtering sensory input, leading to numbness or disconnection. When this happens, clients may appear “spacey” or detached, per Lanius et al. (2001).
Applying Neuroscience to Trauma Therapy
Understanding the thalamus’s role can transform your approach. Research has shown that Eye Movement Desensitization and Reprocessing (EMDR) activates the thalamus through bilateral eye movements, helping clients better filter sensory information and integrate traumatic experiences (Bergmann, 2008). This reduces the intensity of re-experiencing symptoms by balancing internal and external awareness. Cognitive Behavioral Therapy (CBT) also shows promise, increasing thalamus activation and reducing PTSD symptoms, per Peres et al. (2007). These brain-based strategies can guide your treatment planning, ensuring client-centered care grounded in neuroscience.
Earn CE Credits with Online CE Credits
At Online CE Credits, we offer NBCC- and ASEB-approved courses to deepen your neuroscience-based practice. With over 250 on-demand courses, you can learn 24/7, earning credits at your pace. Explore our trauma-focused CE programs and start transforming your practice today!
Conclusion
The thalamus’s role in sensory processing makes it a key player in trauma therapy. By understanding its impact on PTSD symptoms and leveraging therapies like EMDR and CBT, you can help clients heal more effectively. Explore these insights further with Online CE Credits and take your practice to the next level.