by Sadaqut | Oct 11, 2024 | Educational
As a clinician working with autistic clients, you may encounter unique challenges when implementing traditional therapeutic models, particularly exposure therapy. Exposure-based interventions—designed to help reduce anxiety by confronting feared stimuli—can be highly effective. But they require tailored approaches to meet each client’s distinct needs.
You must understand how autistic traits interact with anxiety and how you can adapt typical methods.
Recognizing the Anxiety-Autism Connection
Individuals with autism often experience heightened levels of anxiety, which can stem from a variety of triggers. In the UK, the National Austic Society’s survey discovered that autistic patients fall into the severe anxiety category 47% of the time, according to GAD diagnostic guidelines.
Sensory overload, changes in routine, and social unpredictability are common sources of distress. This can lead to avoidance behaviors that closely mirror those seen in individuals with anxiety disorders, making exposure therapy a potentially valuable tool.
However, anxiety in autism isn’t always linked to the same triggers as in neurotypical individuals. For instance, what might be a mild nuisance to one person—a bright light or a sudden noise—can feel overwhelming and unbearable to someone with sensory processing difficulties.
As a result, clinicians should identify these individual triggers and customize exposure tasks to reflect the specific experiences of their clients.
Modifying Exposure Therapy Techniques
Practitioners often rely on gradual exposure, where clients are introduced to their fears in increasingly challenging doses. With autistic clients, though, this can sometimes backfire if you don’t consider their sensitivities. Instead of following a standard hierarchy of fear, therapists may need to build personalized exposure plans that reflect the client’s unique sensitivities and their emotional thresholds.
For example, if a client struggles with loud environments, the exposure might start with a recording of background noise at a tolerable level. Over time, the volume can be gradually increased, or the client might be introduced to more complex auditory environments in carefully controlled steps.
You should empower the client to gain control of the exposure process. This can benefit autistic individuals who often struggle with a sense of unpredictability in their daily lives.
The process can take longer than in typical exposure therapy cases, so you need to remain patient and flexible. Rushing the process or pushing clients too quickly can lead to increased anxiety and potentially cause them to disengage from therapy altogether.
Building Trust and Predictability
Predictability is essential when working with autistic individuals. Exposure therapy often involves pushing clients into uncomfortable situations. However, unpredictability can increase anxiety in autistic clients and lead to resistance to therapy.
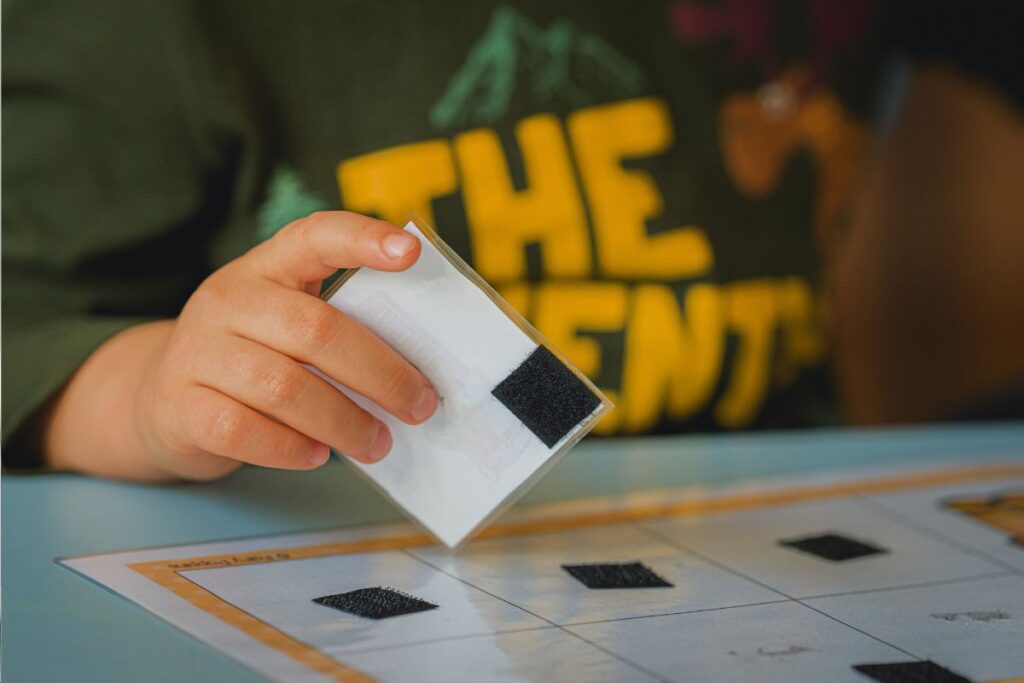
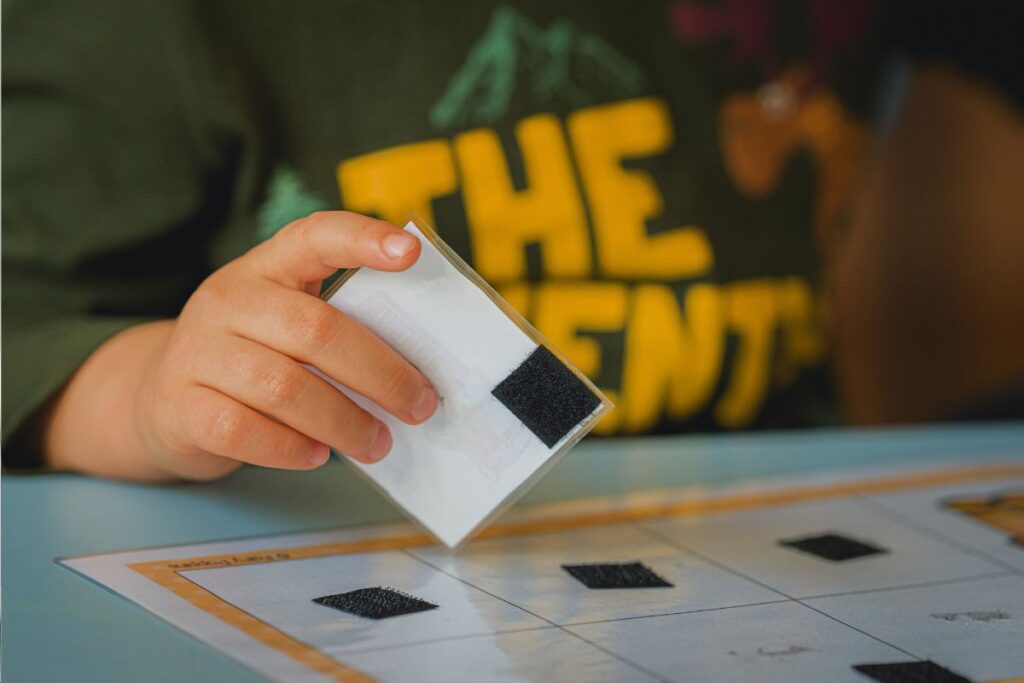
One helpful strategy is to introduce exposure exercises in a highly predictable and structured manner. Clients benefit from knowing exactly what to expect at each stage, and transparency around what each exposure entails can help them feel more secure. For example, you can offer a visual schedule of exposure tasks, breaking down each step in clear and simple terms.
Trust is equally vital. Autistic clients need to feel confident that their therapist understands their unique challenges and will not push them into situations they cannot handle. Establishing this trust from the outset is crucial.
Encourage open communication to enable clients to feel comfortable expressing when they feel overwhelmed or when a particular exposure feels too intense. The therapeutic relationship becomes a collaborative effort where the client’s input is valued and respected.
Sensory Considerations in Exposure Therapy
While exposure therapy traditionally focuses on fear and anxiety, sensory sensitivity requires a different approach. Many autistic individuals have intense reactions to stimuli like light, sound, texture, or movement, and these sensitivities can sometimes be mistaken for generalized anxiety. Understanding the difference between sensory overload and anxiety is crucial in planning effective exposure interventions.
In these cases, exposure therapy can be adapted to focus on sensory desensitization. The goal isn’t to eliminate the sensitivity but to help the individual tolerate it in a way that reduces the intensity of their distress.
For example, a client might work on tolerating the texture of certain fabrics or the sound of a vacuum cleaner by starting with short, controlled exposures and gradually increasing their exposure time.
It’s also important to recognize that sensory sensitivities can vary from day to day. What feels tolerable in one session might be unbearable the next, and therapists should remain attuned to these fluctuations. Flexibility is key, as is the willingness to adjust the pace of therapy as needed.
Adjusting for Communication Styles
Many autistic clients communicate differently from neurotypical individuals, which can sometimes complicate traditional exposure therapy. Nonverbal communication, repetitive speech, or difficulty with emotional expression are common in autism and may require clinicians to adopt alternative communication strategies.
For clients who are less verbal, visual aids can be an excellent tool for explaining exposure tasks and tracking progress. Some clients may respond well to social stories, where therapists create narratives that explain what will happen during exposure exercises in simple, concrete terms.
Others may benefit from using a feelings chart to indicate their emotional state before, during, and after exposure tasks. These charts allow clients to communicate their distress level in a visual way, providing therapists with valuable feedback on how the exposure process is affecting them.
Reinforcing Positive Coping Strategies
For many autistic clients, the strategies they use to cope with anxiety can look very different from those used by neurotypical individuals. Some may rely on repetitive behaviors or “stimming” to self-soothe, while others may prefer deep pressure or quiet time to calm their nervous systems.
Instead of discouraging these behaviors, clinicians can incorporate them into exposure therapy as positive coping mechanisms. For example, if a client engages in hand-flapping or rocking to calm down after exposure to a stressful stimulus, this can be encouraged as a healthy way to manage their anxiety.
Over time, you can help clients expand their repertoire of coping strategies, introducing new methods like breathing exercises or mindfulness practices, but without trying to replace behaviors that are already serving a functional purpose.
Involving Caregivers in the Process
Autistic individuals often benefit from having caregivers involved in their therapy. Family members or support staff can offer valuable insight into the client’s triggers and coping mechanisms, and their participation can help reinforce therapeutic progress outside of sessions.
Mental health professionals should consider involving caregivers in the exposure planning process, especially when it comes to implementing exposure exercises at home. For example, if a child is working on tolerating the noise of a vacuum cleaner, parents can be encouraged to practice short exposures at home, building on the work done in therapy.
However, it’s important to strike a balance between involving caregivers and respecting the client’s autonomy. Having too much outside involvement can feel invasive for autistic patients. So you should always prioritize the client’s preferences and work collaboratively to determine the appropriate level of caregiver involvement.
Alternative Therapies To Treating Autism
Looking to broaden your knowledge about autism interventions? Online CE Credits has a treasure trove of nationally approved courses from seasoned professionals. Browse the programs below to learn more:
Also, consider specialized training in autism to dominate your practice and offer practical interventions to your clients.
Personalizing the Process
The core principles of exposure therapy remain effective for autistic clients, but the process requires careful adaptation to meet their unique needs. By prioritizing trust, predictability, and individualized planning, you can help autistic clients face their fears in a way that feels manageable and empowering.
Adjust your methods and stay attuned to each client’s individual sensory sensitivities, communication style, and preferred coping strategies. With patience and flexibility, exposure therapy can be a powerful tool in reducing anxiety and improving the quality of life for individuals with autism. Also, upgrading your knowledge about autism therapy is a great step towards your career development.

by Sadaqut | Oct 11, 2024 | Certificate
Prolonged Exposure Therapy (PE) is an established, research-backed method for treating Post-Traumatic Stress Disorder (PTSD). As a mental health professional, gaining expertise in this approach can be transformative for client outcomes, especially for individuals dealing with trauma-related symptoms.
This article will explore essential techniques, practical insights, and key training elements of PE therapy to enable you to offer effective care to your clients.
The Basics of Prolonged Exposure Therapy
Dr. Edna Foa developed PE therapy, and it’s grounded in cognitive behavioral principles. The method is based on the idea that avoidance maintains PTSD symptoms. When individuals avoid trauma reminders or memories, their fears remain unprocessed. PE works by encouraging clients to gradually confront these fears, allowing them to process the traumatic memory and reduce their emotional response.

In PE, clients are encouraged to relive their trauma memory in a controlled environment through a process called “imaginal exposure” and to face real-life situations they’ve been avoiding, referred to as “in vivo exposure.” Both forms of exposure allow the brain to reprocess the traumatic memory in a way that reduces its power over time.
Importance of PE Training
For mental health professionals, having proper PE training is crucial. Without the right understanding of its structure and techniques, it’s easy to misapply the treatment, leading to negative experiences for clients. It’s also essential for therapists to know how to manage the emotional intensity that arises during sessions.
Training in PE not only sharpens clinical skills but also ensures that clients are safely and effectively guided through their recovery process.
Core Techniques of Prolonged Exposure Therapy
Prolonged Exposure Therapy consists of several key techniques that therapists must become familiar with during their training:
Imaginal Exposure
Imaginal exposure is perhaps the most important element of PE. This involves asking clients to recount their trauma memory in detail, in the present tense, as if they are reliving the event. The therapist guides this process in a way that helps the client stay in the experience long enough for emotional processing to occur.
Clients typically do this exercise in session, and the therapist will ask them to revisit the memory multiple times, with the goal of reducing emotional arousal. Sessions are recorded, and clients are asked to listen to the recordings between sessions to further desensitize themselves to the trauma memory.
Training therapists in this technique involves learning how to structure imaginary exposure sessions, guiding clients through difficult emotions, and assessing when it’s appropriate to push further or pull back. The practitioners tone, pacing, and ability to create a supportive space are key components in this process.
In Vivo Exposure
In vivo exposure involves confronting real-life situations that the client has been avoiding due to their trauma. For example, someone who experienced a car accident might avoid driving. The therapist and client will work together to create a list of situations called a “fear hierarchy,” ranging from mildly distressing to highly distressing.
Clients are encouraged to face these situations in a gradual way, moving up the hierarchy as their anxiety diminishes. It’s important for mental health professionals to help clients identify these situations and ensure that they are approached with appropriate pacing. PE training equips therapists with strategies to balance challenge and safety, helping clients face their fears without becoming overwhelmed.
Processing and Reflection
After each exposure exercise, whether imaginary or in vivo, the practitioner engages the client in processing what happened during the exposure. This involves asking open-ended questions that help clients reflect on their emotional and physical reactions. It’s not uncommon for clients to experience new insights about their trauma, which helps them reinterpret their experience in a way that’s less threatening.
PE training focuses heavily on helping clinicians learn how to guide these post-exposure discussions. It’s important for therapists to understand the emotional arc of the exposure and enable clients to recognize the progress they’re making, even if it feels uncomfortable in the moment.
PE Training: What To Expect
For those interested in becoming proficient in PE, there are a variety of training programs available. These range from basic workshops to intensive certifications, often provided by institutions specializing in trauma treatment or cognitive-behavioral therapy.
Training typically involves a mix of didactic instruction, role-playing, and supervised practice. Trainees are expected to practice the techniques in controlled environments, and in some cases, they might be asked to treat actual clients under supervision. Learning how to handle client anxiety and discomfort is a big part of the training. You can learn how to manage sessions in which clients become emotionally dysregulated or resistant to the process.
One valuable aspect of PE training is the emphasis on self-awareness. Health professionals are encouraged to monitor their own emotional reactions during sessions. This is because working with trauma can be intense and triggering for therapists, too. Developing skills for self-care and emotional regulation is a vital part of any good PE training program.
Research Supporting PE’s Effectiveness
Prolonged Exposure Therapy’s effectiveness has been well documented through numerous studies and clinical trials. Research has consistently shown that PE can significantly reduce PTSD symptoms in a variety of populations, including combat veterans, survivors of sexual assault, and individuals affected by natural disasters.
One of the most compelling aspects of PE is its versatility. It has been adapted for use with different cultural groups and can be delivered in individual, group, or even virtual formats. For therapists, this adaptability means that training in PE opens doors to serving a broad range of clients, making it a highly practical and impactful treatment modality to add to one’s skill set.
Practical Applications in a Clinical Setting
When implementing PE in practice, you need to strike a balance between structure and flexibility. Although PE is structured therapy with specific protocols, you should be attuned to the individual needs of each client. For instance, some clients might progress quickly through their fear hierarchy, while others may need more time. Likewise, certain trauma memories may be harder to engage with than others.
The PE therapist is prepared to handle these nuances, tailoring the treatment to meet the client where they are. This requires not only mastery of the techniques but also a strong therapeutic alliance, which is critical for clients to feel safe enough to engage in the emotionally intense work of trauma processing.
Another key to successful PE implementation is regular assessment. Clinicians must continually evaluate client progress to ensure the exposure exercises have the desired effect of reducing trauma-related distress.
If the client’s symptoms are not improving, you may need to adjust the treatment plan. PE training teaches therapists how to assess progress effectively and how to modify the therapy if it’s not producing the expected results.
Why Pursue PE Training?
PE training offers a concrete way to help clients move forward in their healing process. Unlike some therapies that rely heavily on insight or discussion, PE is an active, results-driven approach that focuses on doing. This can be incredibly empowering for clients who have felt stuck in their trauma for years.

Also, the evidence base supporting PE means that clinicians can feel confident about using a treatment with a high success rate. The intervention stands out as a proven intervention in a field where some therapies lack strong research backing. Investing time in training is a step toward providing clients with the best possible care.
Consider Other PSTD Therapy Interventions
Since PE also deals with PTSD, you can brush up your skills in other relevant therapies to empower your clients to recover from the mental health condition. Here are some modern courses to consider:
Take Advantage of PE To Manage PTSD
In summary, Prolonged Exposure Therapy offers an effective, evidence-based approach to treating PTSD. Training can equip you with powerful tools to help clients confront and process their trauma. Through the use of imaginal and in vivo exposures, you can guide clients toward significant improvements in their symptoms, providing hope for a brighter future. And you can partner with Online CE Credits to enhance your PE therapy skills today!

by Sadaqut | Oct 11, 2024 | Educational
Narrative Exposure Therapy (NET) is an evidence-based approach that offers a structured yet flexible way of helping individuals process trauma. As a mental health professional, adding NET to your skill set can provide substantial benefits to your trauma care practice. It’s ideal for clients with complex trauma histories, such as refugees, survivors of war, or individuals with chronic childhood abuse.
NET is grounded in storytelling, encouraging clients to narrate their life experiences within a chronological structure. This not only helps them organize traumatic memories but also aids in integrating those experiences into their broader life narrative.
Understanding the NET Approach
In many trauma-focused therapies, the goal is to help clients reprocess traumatic events to reduce symptoms of PTSD and other related conditions. NET takes a unique approach by focusing on creating a coherent autobiographical timeline of the client’s life. The client is encouraged to explore both positive and traumatic experiences, situating their memories within their overall life story.

NET follows a structured format where clients recount their memories in chronological order, focusing particularly on the most intense or distressing events. This helps clients face traumatic memories while emphasizing that these events are part of a larger, more complex life narrative. Through this process, NET seeks to transform fragmented, disorganized memories into a more cohesive story.
The therapist guides the client through this journey, helping them not only recount their trauma but also place it within the broader arc of their lives. This allows for both emotional processing and cognitive restructuring, helping individuals understand their trauma as just one part of their life experience rather than the defining feature.
Why NET Is Effective for Trauma Treatment?
NET’s effectiveness lies in its simplicity and focus on narrative coherence. Many clients who experience complex trauma struggle with fragmented memories and disorganized thoughts about their past. So storytelling helps to bridge these gaps. By encouraging clients to recall events in order, the therapy supports emotional processing in a way that makes the memories less overwhelming.
From a neurological standpoint, NET helps by reducing the emotional charge of traumatic memories. Over time, retelling these memories in a safe therapeutic environment can make them less distressing and intrusive. This process helps to reduce symptoms of PTSD, such as flashbacks, nightmares, and hyperarousal.
Additionally, NET promotes resilience by highlighting the client’s strengths and positive memories. When trauma dominates a person’s mind, it’s easy for them to overlook positive aspects of their life. NET encourages clients to remember and integrate these positive experiences, which can enhance their overall emotional well-being and self-worth.
How NET Fits Into Trauma Care
One of the key benefits of NET is its structured yet adaptable format. If you’re used to trauma-focused approaches like Cognitive Behavioral Therapy (CBT) or Eye Movement Desensitization and Reprocessing (EMDR), you might find NET to be a valuable addition to your toolbox. It works with clients who have multiple, layered trauma experiences.
One of the core principles of NET is that it’s helpful for individuals who have experienced ongoing, repeated trauma. Many therapies, while effective, are more suited for single-event trauma. NET, by contrast, is well-suited to clients who have been exposed to prolonged trauma, such as survivors of conflict, forced migration, or childhood abuse. By organizing these experiences into a timeline, the therapy allows for the processing of multiple traumatic events, giving clients a sense of control over their past.
The Process of Becoming Trained in NET
If you’re interested in incorporating NET into your practice, training is accessible and can often be completed over the course of a few days. The training typically covers the basic principles of the therapy, including how to structure sessions, work with traumatic memories, and create the life narrative with your client.
The initial training gives you the foundational skills to begin using NET in your practice, but many professionals choose to continue refining their skills through supervision or advanced workshops.
A particularly valuable aspect of NET training is the focus on cultural competence. Given that NET has been used extensively with refugees and survivors of war, the training often emphasizes how to work with clients from diverse cultural backgrounds. This makes it especially useful for therapists who work in multicultural settings or with clients from marginalized populations.
Real-World Application: Bringing NET Into Your Practice
Once trained, many therapists find that NET can complement other forms of trauma therapy. For example, if you’re working with a client who struggles to make sense of their traumatic experiences, incorporating NET can provide a way to organize those memories into a more coherent whole.

The therapy can be especially useful for clients who find it difficult to talk about their trauma in detail, as the structured nature of NET provides a sense of containment and safety.
Many therapists also report that NET helps improve therapeutic rapport. By working with clients to tell their story, therapists can foster a sense of collaboration and mutual trust. This can be particularly helpful when working with clients who have had difficulty opening up in other therapeutic settings.
Incorporating NET into your practice doesn’t mean you need to abandon other techniques you use. Many professionals find that NET works well alongside other therapies, such as EMDR or Trauma-Focused Cognitive Behavioral Therapy (TF-CBT). For instance, you might use NET to help a client organize their traumatic memories and then use EMDR to process particularly distressing memories in more depth.
The flexibility of NET allows it to be adapted to your specific clinical style and the unique needs of your clients. For those working in community mental health settings or with underserved populations, NET can be especially useful because it is designed to be brief and effective even in low-resource settings. This makes it an ideal choice for therapists who may not have the luxury of long-term therapeutic interventions with their clients.
Expanding Your Trauma Care Practice With NET
Expanding your skill set to include NET opens up new opportunities for working with diverse populations. Whether you’re working in private practice, a community clinic, or a humanitarian setting, NET provides a structured and effective way to help clients process trauma. The emphasis on narrative allows clients to reclaim their story, offering a sense of agency and control that is often lost in the aftermath of trauma.
NET also offers a powerful way to help clients integrate their experiences into a coherent and manageable narrative. By incorporating this therapy into your practice, you can offer a more structured, client-centered approach to trauma care that addresses both the emotional and cognitive aspects of trauma. For clients who have been through significant, complex traumas, this approach can make a world of difference in their journey toward healing.

by Sadaqut | Oct 11, 2024 | Educational
Solution-Focused Therapy (SFT) is a strengths-based approach that helps clients envision their preferred future and identify the steps needed to achieve it. Unlike some therapeutic methods that focus heavily on analyzing problems, SFT shifts the focus to solutions, resources, and the client’s existing strengths. This method often proves effective for clients who want to make tangible progress in a relatively short time.
Get up to speed with SFT to hone your skills and earn 2.5 credits effortlessly.
Let’s explore several essential SFT questions that drive client engagement and facilitate meaningful change.
The Miracle Question: Envisioning the Future
The Miracle Question is perhaps one of the most well-known tools in SFT. It invites clients to imagine a future where their issues are resolved overnight. This technique helps clients articulate their goals and desires, often in ways they hadn’t previously considered.

“Suppose tonight, while you sleep, a miracle happens and the problem that brought you here is resolved. How would you know that a miracle happened? What would be different?”
This question can help clients shift from a problem-focused mindset to one that is more solution-oriented. They start to visualize a future where they have overcome their current challenges, which can be incredibly empowering.
Scaling Questions: Measuring Progress and Confidence
Scaling questions are used to assess a client’s current position relative to their goals and to identify small, achievable steps for moving forward. These questions are particularly useful for tracking progress over time and for making abstract concepts more concrete.
“On a scale from 0 to 10, where 0 means the problem is the worst it has ever been and 10 means the problem is completely resolved, where do you see yourself today?”
Follow-up questions like, “What would it take to move one step up the scale?” encourage clients to think about specific, manageable actions to improve their situation. Scaling questions not only help in setting realistic goals but also provide a framework for celebrating small victories along the way.
Exception Questions: Discovering What Works
Exception questions help clients identify times when their problem was less severe or when they were able to cope more effectively. These questions are vital for uncovering hidden strengths and resources that the client can use in the present.
“Can you think of a time recently when the problem wasn’t as intense? What was different about that situation?”
By pinpointing these moments, clients can begin to understand what factors contributed to their success during those times. Whether it’s a supportive friend, a particular mindset, or a coping strategy, identifying these exceptions can be key to replicating and building upon past successes.
Coping Questions: Acknowledging Effort and Resilience
Coping questions are particularly helpful for clients who feel stuck or overwhelmed. These questions acknowledge the effort the client is already putting in and validate their ability to manage difficult situations, even if they aren’t seeing significant changes yet.
“How have you managed to keep going, despite the difficulties you’re facing?”
This type of question can open up a discussion about the client’s resilience and the small, perhaps unnoticed ways they are already coping. It shifts the focus from what isn’t working to what is, no matter how small or seemingly insignificant.
Goal-Oriented Questions: Defining Success
Setting clear, concrete goals is a cornerstone of SFT. Goal-oriented questions help clients articulate what they want to achieve in a way that is specific and actionable. This clarity is crucial for both the client and the therapist to work effectively towards achieving those goals.
“What will be the first sign that things are getting better for you?”
This question encourages clients to define success in their own terms, providing a tangible marker to strive toward. Having a clear indicator of progress helps in maintaining motivation and focus throughout the therapeutic process.
Exploring Motivation: What’s at Stake?
Understanding what motivates a client to seek therapy is crucial for tailoring the therapeutic approach to their needs. Questions that explore motivation can help both the therapist and the client understand the deeper reasons for wanting change, which can be pivotal in sustaining effort and engagement.
“What makes this change important to you right now?”
This question can reveal underlying values and priorities, making it easier to align therapeutic interventions with what the client truly cares about. Whether it’s family therapy, personal well-being, or career aspirations, identifying these motivators can significantly enhance client commitment to the process.
Resource Questions: Uncovering Hidden Strengths
Resource questions aim to uncover the internal and external resources the client already possesses. These could be personal traits, supportive relationships, or past experiences that have equipped them to handle challenges.
“When you’ve faced difficulties like this before, what helped you get through it?”
By identifying these resources, clients can begin to see themselves as more capable and resilient. This recognition can be empowering and can serve as a foundation for developing new coping strategies and solutions.
Exploring Small Steps: Incremental Change
Sometimes the path to change can feel overwhelming, and clients may struggle to see how they can get from where they are to where they want to be. Exploring small, actionable steps can make the process feel more manageable.
“What’s the smallest step you can take this week that would move you closer to your goal?”
This question helps clients break down their goals into smaller, more achievable tasks. Taking incremental steps can build momentum and provide a sense of accomplishment, which is crucial for maintaining motivation over time.
Strengths-Based Questions: Highlighting What’s Working
Clients often come to therapy feeling discouraged and may have a negative view of themselves. Strengths-based questions help shift this narrative by highlighting the client’s skills, attributes, and past successes.

“What qualities or strengths have helped you navigate tough times before?”
Acknowledging these strengths can help clients build a more positive self-concept and foster a sense of self-efficacy. This can be particularly important for clients who struggle with low self-esteem or who have difficulty recognizing their own accomplishments.
Future-Oriented Questions: Visualizing the Path Ahead
Future-oriented questions help clients imagine what life could look like once they’ve achieved their goals. This vision can serve as a powerful motivator and provide a sense of hope and direction.
“How will your life be different once you’ve achieved your goals?”
Encouraging clients to think about the positive changes they want to see can help maintain focus and motivation. It also provides a concrete picture of what they are working towards, making the therapeutic process feel more purposeful and directed.
Conclusion: Master SFT Questions To Dominate Your Practice
Incorporating these essential questions into your SFT practice can significantly enhance client engagement and facilitate meaningful progress. Each question serves a distinct purpose, whether it’s helping clients articulate their goals, recognize their strengths, or take actionable steps toward change.
By fostering a collaborative, solution-focused dialogue, therapists can empower clients to become active participants in their own healing process. It can be a valuable tool whether you are new to Solution-Focused Therapy or looking for ways to deepen your practice. Advance your career today and dominate your practice.

by Sadaqut | Sep 27, 2024 | Educational
Intergenerational trauma is not just a passing concern for many mental health professionals. It’s a persistent challenge that can span several generations, affecting families, communities, and entire cultures. Whether stemming from war, systemic oppression, or family violence, this trauma can influence how people relate to each other, how they parent, and how they navigate their personal and social lives.
Recognizing these deep-rooted patterns, the Intergenerational Trauma Treatment Model (ITTM) has been developed to address the needs of those affected, offering a path toward healing and recovery.
The Reality of Intergenerational Trauma
The concept of intergenerational trauma is not new. It refers to the transmission of trauma from one generation to the next. Trauma doesn’t just affect the person who directly experienced it; it can seep into family dynamics, parenting styles, and even genetic makeup.
Trauma survivors’ children often grow up in environments shaped by the emotional and psychological wounds of their parents, even if the original trauma occurred decades ago.

For example, children who have grown up in families affected by slavery or genocide often exhibit signs of trauma, even without direct exposure to the events themselves. The trauma can manifest in a variety of ways, such as anxiety, depression, difficulties in forming relationships, or a pervasive sense of fear or distrust.
This kind of trauma is complex because it’s often intertwined with cultural, historical, and familial contexts, making it challenging to treat through traditional methods.
Embrace Several Therapy Interventions To Treat Intergenerational Trauma
Mental health professionals such as psychiatrists, psychologists, and other physicians are concerned about the effect of intergenerational trauma. So does Online CE Credits, a therapist-managed platform with the most up-to-date trauma treatments. The online courses empower you to apply emerging trauma techniques to help your clients heal.
Take a look at the accredited courses below:
The Need for a Specialized Treatment Approach
Intergenerational trauma requires a specialized approach that goes beyond individual therapy. While traditional therapy can address personal experiences of trauma, it may fall short in recognizing and treating the ways trauma is passed down through families and communities.
The ITTM is designed specifically to address these unique challenges by focusing not just on the individual but also on their family and community context.
The model acknowledges that healing needs to occur on multiple levels. It’s not enough to address the trauma in the person sitting in the therapist’s chair. Instead, ITTM seeks to understand the broader picture—how family dynamics, community relationships, and cultural histories all contribute to the perpetuation of trauma.
The goal is to break the cycle of trauma transmission and help individuals and families create new, healthier patterns.
Core Components of the Intergenerational Trauma Treatment Model
The ITTM integrates several therapeutic approaches to provide a comprehensive treatment plan. These include:
Family Therapy:
Since trauma often affects entire families, therapy sessions that include multiple family members can be crucial. Family therapy within the ITTM framework helps families understand the origins of their struggles and how trauma has influenced their relationships.
This kind of therapy is vital for uncovering and addressing unhealthy patterns that may have been passed down from generation to generation.
Narrative Therapy:
Encouraging individuals and families to share their stories is a powerful tool in the healing process. Narrative therapy allows people to reframe their experiences, helping them see themselves not as victims of their past but as survivors with the strength to create a different future.
This aspect of ITTM is particularly important for communities where silence and secrecy around trauma have been prevalent, giving voice to those who have been historically silenced.
Cultural Sensitivity:
The ITTM recognizes that culture plays a significant role in how trauma is experienced and transmitted. Treatment plans are therefore tailored to respect and incorporate cultural beliefs and practices.
This can involve working with community leaders, understanding cultural rituals and traditions, and acknowledging the specific historical and cultural contexts that have contributed to the trauma.
Psychoeducation:
Educating clients about the nature of trauma and its effects is a fundamental part of ITTM. Understanding how trauma impacts the brain, body, and behavior can be incredibly empowering for clients. This knowledge helps them make sense of their experiences and realize that their reactions are normal responses to abnormal circumstances.
Interventions for Children and Adolescents:
Children and adolescents who grow up in traumatized environments need age-appropriate specialized interventions sensitive to their developmental stages. ITTM includes strategies such as play therapy, art therapy, and trauma-focused cognitive-behavioral therapy (TF-CBT) to help young people process their experiences in a safe and supportive environment.
Community-Based Approaches:
Healing doesn’t happen in isolation. ITTM often involves community-based approaches that foster a sense of belonging and collective healing. This can include group therapy sessions, community workshops, and cultural healing practices that bring people together to share their experiences and support one another.
The Role of Therapists in ITTM
Therapists working within the ITTM need to be particularly attuned to intergenerational trauma’s complex dynamics . This requires them to combine clinical expertise, cultural competence, and a deep understanding of family systems. Health professionals must be able to hold space for clients as they explore painful and often deeply buried emotions.
They also need to be skilled in helping clients recognize and disrupt unhealthy patterns of behavior that have been passed down through generations.
Also, practitioners must be aware of their own potential biases and the ways in which their own cultural backgrounds may influence their understanding of trauma. Continuous training and supervision are essential for therapists working with intergenerational trauma to ensure they provide the most effective and sensitive care possible.
Challenges and Considerations in ITTM
While ITTM offers a promising approach to healing intergenerational trauma, it’s not without its challenges. One of the primary difficulties is the deeply entrenched nature of intergenerational trauma. Breaking the cycle requires not just time and effort but also a willingness to confront painful family histories and cultural legacies. This process can be emotionally exhausting for both clients and therapists.
In addition, factors such as the availability of culturally competent therapists, access to resources, and the level of support within the community can influence ITTM’s effectiveness. In some cases, there may be resistance to addressing trauma, particularly in cultures where discussing such issues is taboo.
Overcoming these barriers requires a sensitive and patient approach, as well as a strong commitment to the long-term process of healing.
Moving Forward: The Future of Intergenerational Trauma Treatment
The Intergenerational Trauma Treatment Model represents a significant step forward in our understanding of how trauma is transmitted across generations and how it can be treated. ITTM breaks the cycle of trauma transmission by addressing trauma on multiple levels—individual, family, and community—and paves the way for a healthier, more resilient future.

Mental health professionals working with intergenerational trauma require a deep commitment to learning, cultural sensitivity, and ongoing professional development. As our understanding of trauma continues to evolve, the ITTM will likely continue to adapt and grow, incorporating new research and therapeutic techniques.
However, what remains constant is the model’s emphasis on healing individuals, families, and communities.
Consider ITTM To Treat Complex Trauma
The ITTM is not just a treatment model—it’s a pathway to healing that honors the complex and multifaceted nature of trauma. Intergenerational trauma survivors have hope for a future without the burden of their past.
And therapists can use the model to make a profound difference in their clients by helping them break free from trauma cycles that have held them captive for far too long.
Want to fine-tune your trauma interventions? Partner with Online CE Credits by creating an account today.